
Over the follow-up period there was not only a fall in mean HbA 1c but also a narrowing of the distribution of HbA 1c ( Figure 1), with a lower proportion of high outliers: there were significantly fewer people with HbA 1c levels of ≥80 mmol/mol (seven people at 6 months compared with 24 at baseline). The greatest HbA 1c reduction at 6 months was by 87 mmol/mol. The mean pre-intervention HbA 1c was 83.0 mmol/mol (95% confidence interval, 79.2–86.7). One of the 92 individuals was on a mixed insulin regimen and three were on an insulin pump. Baseline demographics are detailed in Table 1. The mean cohort age was 43 years for men and 39 years for women (overall range, 17–83 years) 42 (45.7%) of the participants were female. All individual patient data were anonymised prior to statistical analysis. Ethics approval was not obtained for this study as the intervention was part of standard care according to NICE (2015) guidance. Kernel density estimation is a fundamental data-smoothing solution in which inferences about the population are made based on a finite data sample. Kernel density estimation was used to compare HbA 1c levels achieved at baseline, 3 months and 6 months. Multiple linear regression was employed to explore the predictors of HbA 1c. None of the participants attended an expert patient programme during the follow-up period or had attended such a programme in the previous 12 months. Most changes made were in the dose rather than the type of insulin. BMI was recorded at the time of initiation of monitoring. HbA 1c was recorded at baseline and 3 months after the start of monitoring in all users, and after 6 months in the majority of users. HbA 1c was measured using the Menoarini autoanalyser (Menarini Diagnostics UK, Wokingham, Berkshire).

An HbA 1c of 60 mmol/mol (7.6%) was taken as the threshold for suboptimal glycaemic control. Initiation took place with education and support from one of the DSNs. We report the outcomes of 92 consecutive adults (18 years of age or more) with type 1 diabetes who have begun using the FreeStyle Libre monitor. We report here the outcome of deploying this technology. Three individuals have declined to use the device when it was offered to them. The device is offered according to NICE NG17 guidance (NICE, 2015). Since Spring 2018, the DSN team has been offering the FreeStyle Libre flash glucose monitor for type 1 diabetes management. The specialist service sees people with type 1 diabetes in an episodic care model in which, once glycaemia has been stabilised, the person with diabetes is again looked after in primary care. There are at least 1000 people known to have type 1 diabetes in Eastern Cheshire, of whom the majority are managed in primary care.

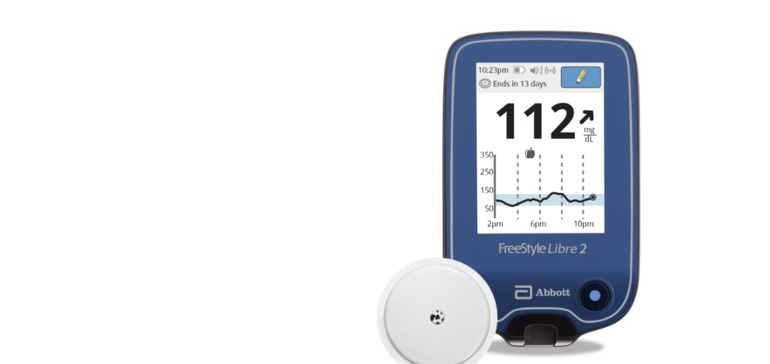
They provide an outreach service to GP practices across the area, as well as clinics at a central location. The DSN team in Eastern Cheshire work across a mixed urban and rural catchment area south of the conurbation of Greater Manchester. In this article, we describe how use of the FreeStyle Libre flash monitor has improved the glycaemic control of many people with type 1 diabetes where the new technology has been intensively deployed. In the area of Eastern Cheshire, UK, the diabetes specialist nurse (DSN) team has been an early adopter of flash glucose monitoring. The glucose data are made available when the user chooses to swipe the reader over the sensor which, in the case of the FreeStyle Libre monitor, remains in place for up to 14 days.ĭespite major advances in the pharmacological management of type 1 diabetes in recent years (Iqbal et al, 2018) and increasing access to expert patient programmes, many people with type 1 diabetes have continued to run high HbA 1c levels (Anderson et al, 2012 Heald et al, 2018). Use of CGM is associated with a reduction in HbA 1c (Pickup et al, 2011).įlash glucose monitoring, in contrast to CGM, does not provide real‐time data with alerts and alarms (Kalra and Gupta, 2015), but allows users retrospectively to review the preceding 8 hours of continuous glucose data, along with a contemporary estimated blood glucose value and trend line.

Continuous glucose monitoring (CGM) devices display an estimate of blood glucose levels, along with trends in direction, in real time, and in the eyes of many they are proving to be a step change in diabetes management. The achievement of better glycaemic control remains a challenge for people with type 1 diabetes and their healthcare professionals.


 0 kommentar(er)
0 kommentar(er)
